Regarding Coronary Microvascular Dysfunction
Table 1 shows the classification of coronary microcirculatory disorders proposed by Crea and Camici. Type 1 originates in the coronary microvessels and is not associated with myocardial disease or obstructive coronary artery disease. “Microvascular angina” is classified here. Type 2 occurs in conjunction with myocardial disease, and Type 3 occurs in conjunction with obstructive coronary artery disease; the nature of these conditions remains largely unexplained. Type 4 is iatrogenic, arising from procedures such as coronary interventions. Details regarding this type also remain unclear. This research group will initially focus on Type 1, but plans to elucidate Types 2–4 in the future.
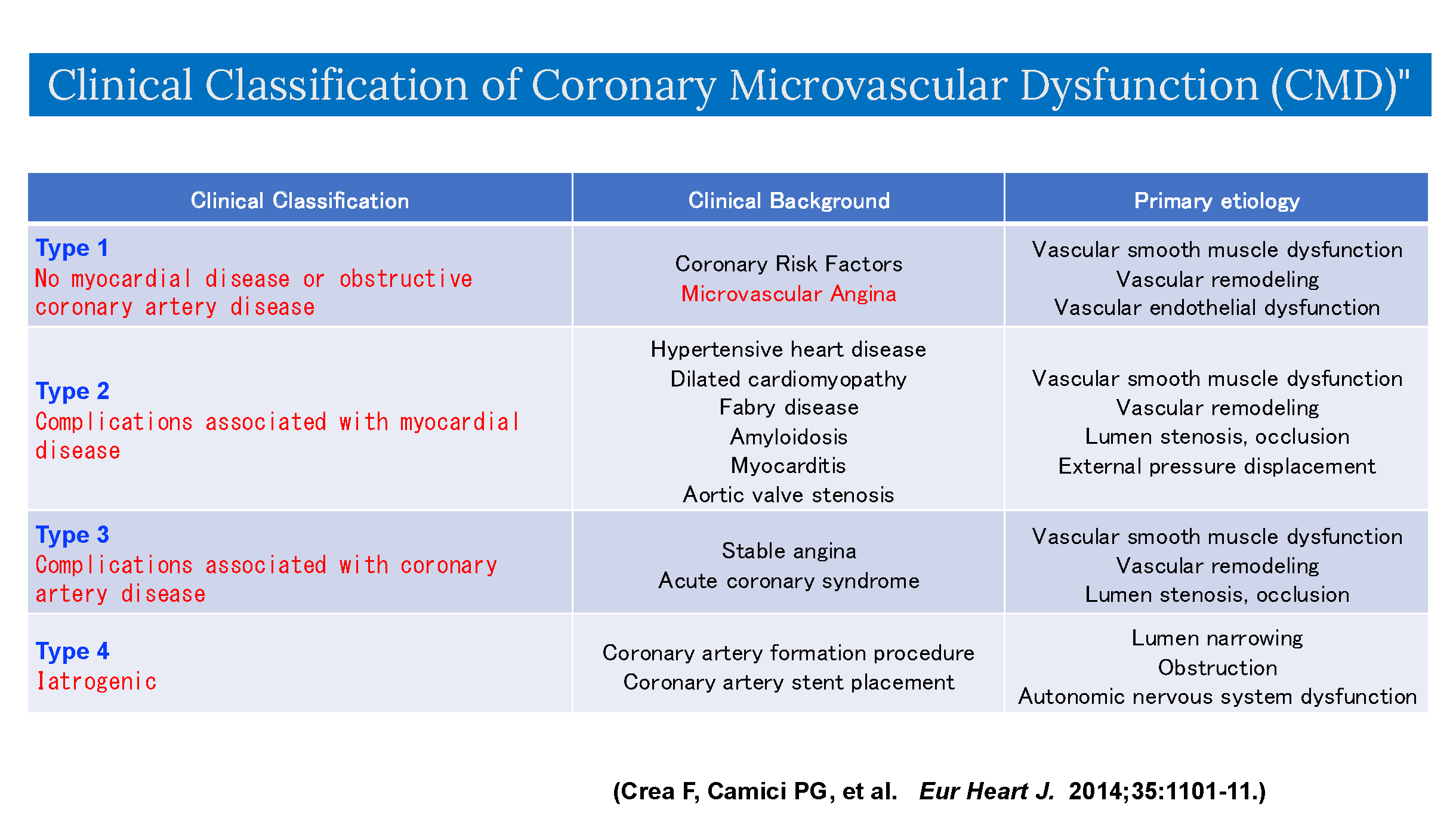
Table 1: Clinical Classification of Coronary Microvascular Dysfunction (CMD)
The condition known as INOCA (ischemia with non-obstructive coronary arteries) has gained attention in recent years. It refers to a state where patients exhibit angina symptoms and show signs of ischemia on non-invasive tests, yet coronary angiography reveals no stenotic lesions in the coronary arteries. INOCA is thought to involve two pathologies: coronary vasospasm and coronary microvascular dysfunction. Regarding coronary vasospasm, if symptoms suggestive of vasospasm are present—such as chest pain in the early morning or during hyperventilation—coronary angiography should be performed. A definitive diagnosis can be made using coronary vasospasm provocation tests with acetylcholine or ergonovine. Regarding the diagnosis of angina due to coronary microcirculatory dysfunction, diagnostic criteria have been published by the Coronary Vasomotion Disorders International Study Group (COVADIS), an international research organization of which Professor Shimokawa, the representative of this study group, is a founding member (Table 2; Reference 8). According to these criteria, the presence of coronary microvascular dysfunction is indicated as a diagnostic requirement, in addition to symptoms of myocardial ischemia, non-obstructive coronary artery disease, and proof of myocardial ischemia. The frequency of coexistence between large coronary artery spasm and microcirculatory dysfunction was reported by Tohoku University (). Among 187 cases suspected of INOCA, 128 cases (68%) had large coronary artery spasm, and 22 cases (12%) were diagnosed with microvascular spasm. Furthermore, reduced CFR was observed in 66 cases (35%), elevated IMR in 70 cases (37%), and 84 cases (45%) exhibited two or more coronary dysfunction abnormalities concurrently (Figure 7).
Therefore, when angina is suspected but no organic stenosis of the large coronary arteries that could explain the angina is found on cardiac catheterization, hastily attributing the cause of symptoms to non-cardiac factors carries the risk of inadequate diagnosis and treatment.
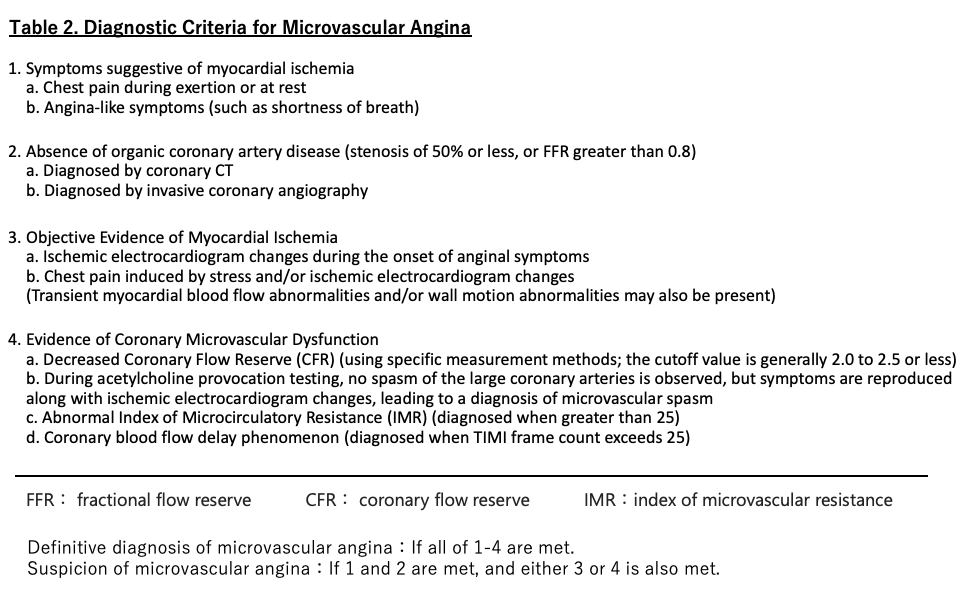

Figure 7. Coexistence of Coronary Artery Dysfunction (Modified from Reference 6): Among 187 cases suspected of angina pectoris who underwent coronary angiography and showed no organic coronary stenosis, 128 cases (68%) were diagnosed with coronary surface spasm based on acetylcholine provocation testing. Regarding the assessment of coronary vasomotor dysfunction, 66 cases (35%) exhibited a decrease in coronary flow reserve (CFR), and 70 cases (37%) showed an increase in index of microcirculatory resistance (IMR). Additionally, 84 cases (45%) presented with two or more types of coronary artery dysfunction, including coronary surface spasm, decreased CFR, and increased IMR.
Approximately 6% of cases clinically diagnosed as acute myocardial infarction based on ECG changes, symptoms, and elevated myocardial enzymes (troponin) show no significant obstructive coronary artery lesions on coronary angiography (Reference 9). This condition is termed MINOCA (myocardial infarction with non-obstructive coronary arteries). To diagnose MINOCA, conditions causing myocardial damage other than ischemia (e.g., myocarditis, takotsubo cardiomyopathy) must be excluded. When MINOCA is suspected, one must first consider the possibility of non-ischemic myocardial damage, followed by careful evaluation for other conditions causing troponin elevation (e.g., pulmonary embolism, sepsis). Furthermore, even if coronary angiography shows no significant stenosis, ① plaque rupture may have occurred, and intravascular imaging (OCT or IVUS) can sometimes visualize unstable plaque. Additionally, ② performing coronary spasm provocation tests along with CFR and IMR measurements can reveal ischemic mechanisms such as coronary spasm or microvascular dysfunction, potentially identifying the cause of MINOCA. Identifying the cause of MINOCA is crucial. If plaque rupture is confirmed, appropriate treatment options like antithrombotic therapy or statins can be selected for each individual case. If coronary spasm is the cause, calcium channel blockers may be indicated. Considering coronary microcirculatory dysfunction as a cause of MINOCA is important. An international report studied 80 consecutive MINOCA cases undergoing coronary spasm induction tests during the acute phase. Positive findings were obtained in 46% of cases, with 65% of these representing spasm in large coronary arteries and 35% representing microvascular spasm (Reference 10).
Takotsubo cardiomyopathy is a condition characterized by diffuse wall motion abnormalities centered on the left ventricular apex and compensatory hypercontractility of the basal region, earning its name “takotsubo” (octopus pot) due to its shape. While generally understood as a reversible condition with a favorable prognosis, reports exist of serious complications such as cardiac rupture and life-threatening arrhythmias. Currently, several mechanisms are considered potential causes of takotsubo cardiomyopathy: 1. multi-vessel coronary spasm, 2. coronary microvascular spasm, and 3. myocardial injury due to catecholamines. It is believed that these pathologies coexist rather than a single cause being responsible. In cases of takotsubo cardiomyopathy, coronary angiography performed during the acute phase may reveal delayed contrast enhancement even in the absence of significant stenosis in the large coronary arteries, suggesting coronary microcirculatory dysfunction. This is thought to be due to factors such as sympathetic hyperactivity, microvascular spasm, and oxidative stress. Numerous aspects of the pathogenesis of this disease remain unclear. Therefore, it is necessary to accumulate and examine cases of takotsubo cardiomyopathy in clinical practice, evaluating coronary microcirculation using methods such as CFR and IMR measurement.
Coronary microcirculatory dysfunction is thought to be deeply involved in the pathophysiology of heart failure with preserved ejection fraction (HFpEF). While reports on the association between CFR (coronary flow reserve), which reflects microcirculatory dysfunction, and HFpEF are scarce, the Eur Heart J 2018;39: 840-849 (Reference 11) measured CFR in 201 consecutive HFpEF patients. The CFR-reduced group (CFR < 2, n=108) had worse prognosis compared to the CFR-normal group. CFR values showed a positive correlation with tissue Doppler-measured e` and a negative correlation with E/e`. Multivariate analysis revealed that reduced CFR was associated with diastolic dysfunction and correlated with both composite cardiovascular outcomes and HFpEF hospitalization. The combination of reduced CFR and diastolic dysfunction (E/e` > 15) was shown to increase the risk of HFpEF-related heart failure hospitalization more than fivefold (Figure 8). This study clearly demonstrated that coronary microcirculatory dysfunction is closely involved in the pathophysiology and prognosis of HFpEF.
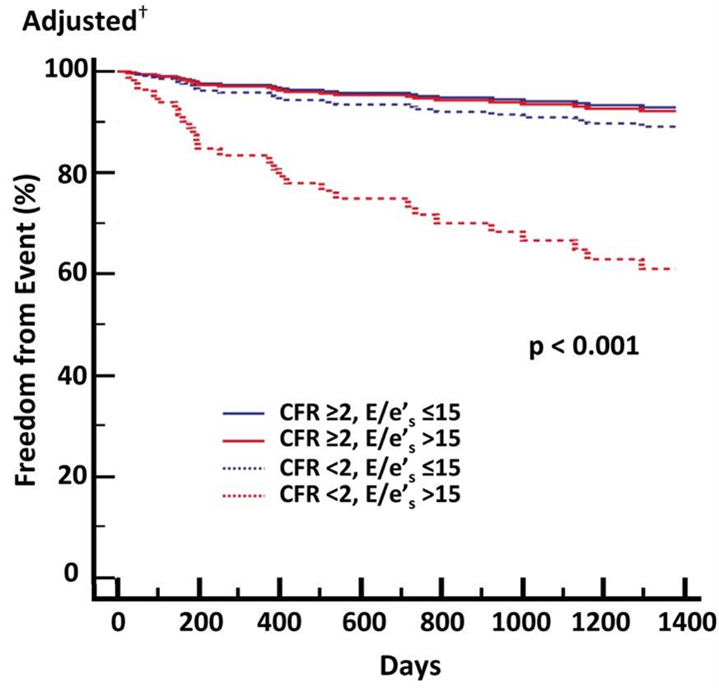
Figure 8 Prognosis of HFpEFPatients According to CFR and Myocardial Diastolic Dysfunction Status (Cited from Reference 11): It was shown that the risk of heart failure hospitalization due to HFpEFincreases more than fivefold when both decreased CFR (less than 2) and diastolic dysfunction (E/e' > 15) are present.
References
6)J Am Coll Cardiol 2019;74(19):2350-60
8)nt J of Cardiol 2018;250:16 -20
9)Circulation 2015;131:861-70
10)Eur Heart J 2018;39:91-98
11)Eur Heart J 2018;39:840-849
© 2022 日本冠微小循環障害研究会